The Role of Diabetes in Pancreatic Cancer: Understanding the Connection
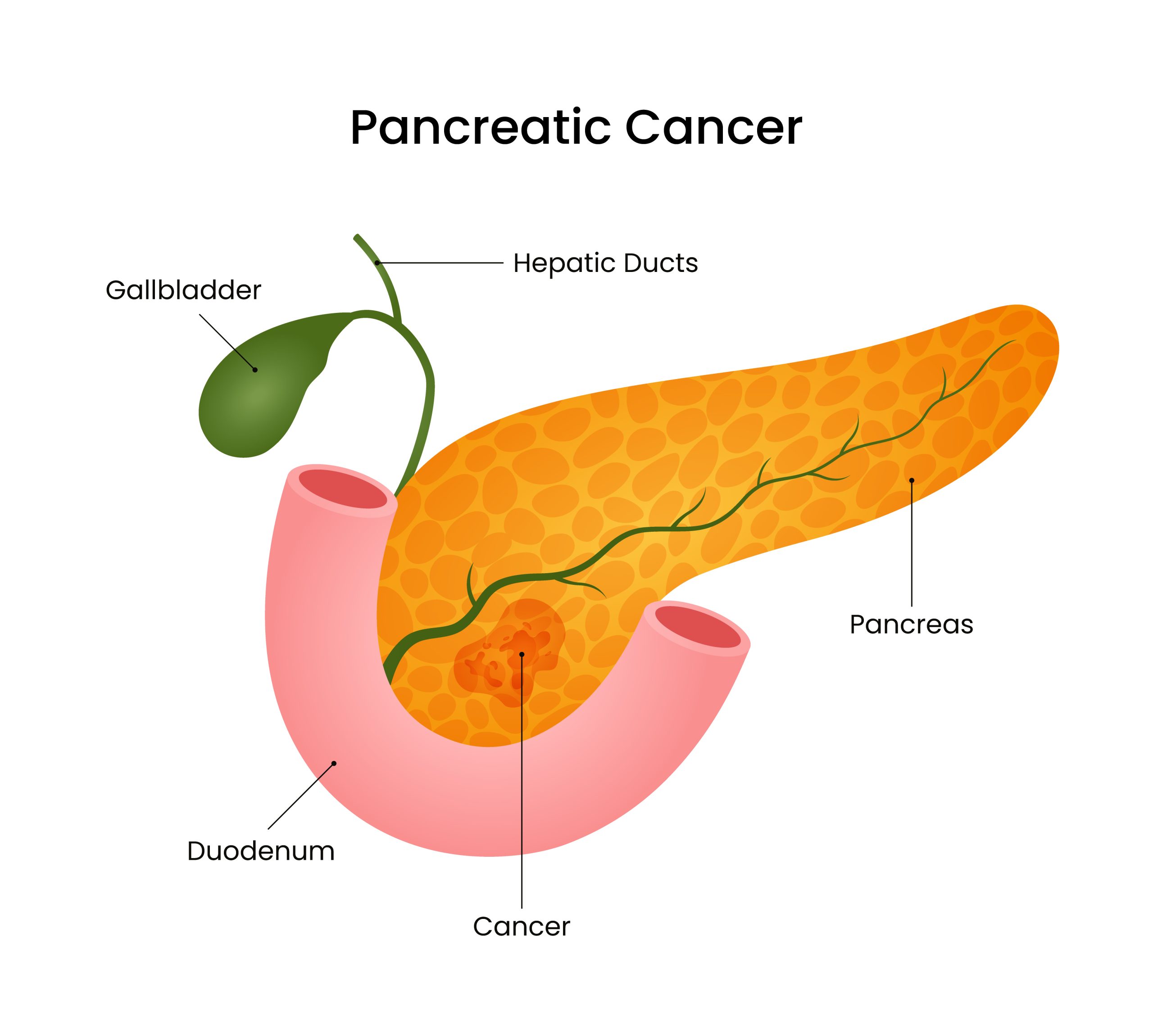
Pancreatic cancer is one of the most aggressive and deadliest forms of cancer, often diagnosed at an advanced stage when cancer treatment options are less. Among the many risk factors associated with pancreatic cancer, diabetes has emerged as a significant and complex one. The relationship between diabetes and pancreatic cancer is complicated, as diabetes can both increase the risk of developing pancreatic cancer and, in some cases, be a consequence of the disease. Let’s explore how diabetes influences pancreatic cancer risk and what this means for patients and healthcare providers.
Is Diabetes a Risk Factor for Pancreatic Cancer?
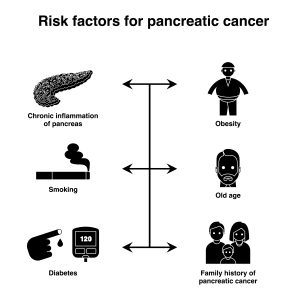
Diabetes has been repeatedly linked to an increased risk of pancreatic cancer, according to research, as compared to those without diabetes. The high risk is especially pronounced in people who have had diabetes for a long time. It is estimated that diabetes can double the likelihood of developing pancreatic cancer, with the risk being even more substantial in people who are obese or have a family history of pancreatic cancer.
Type 2 diabetes, the more common form of diabetes, is mainly associated with an elevated risk of pancreatic cancer illness. Prolonged high blood sugar levels and insulin resistance, which characterize type 2 diabetes, can lead to an inflammatory environment in the body. This inflammation, along with the continuous stimulation of insulin production, is thought to contribute to cancerous changes in the pancreas. Insulin is a growth-promoting hormone, and excessive insulin production over time may encourage the growth of cancer cells in the pancreas.
The Role of Insulin Resistance:
The ineffective response of the body’s cells to insulin is known as insulin resistance, a hormone that pancreas produces that regulates blood sugar levels. Therefore, the pancreas needs to produce more insulin to maintain normal blood sugar levels. The overproduction of insulin can stimulate the growth of pancreatic cells, increasing the potential for mutations and cancer development. Furthermore, insulin resistance is associated with increased levels of insulin-like growth factor (IGF), which can promote cell proliferation and inhibit cell death, further facilitating the growth of cancer cells.

New-onset Diabetes as an Early Indicator:
Interestingly, new-onset diabetes in older adults can sometimes be an early sign of pancreatic cancer rather than just a risk factor. Studies have shown that a significant proportion of people diagnosed with pancreatic cancer had developed diabetes within the previous two to three years. This form of diabetes is often referred to as “diabetes of the exocrine pancreas,” where the cancer interferes with the normal function of the pancreas, disrupting insulin production and causing diabetes.
However, not everyone who develops diabetes later in life will have pancreatic cancer, which poses a challenge for clinicians. Understanding when to investigate further pancreatic cancer in patients with new-onset diabetes remains an area of ongoing research. The goal is to identify which individuals are at the highest risk and could benefit from early screening for pancreatic cancer.

If a diabetic person has pancreatic cancer, should they avoid all sugar?
Well, not unless a doctor or nutritionist advises it. Because cancer cells cannot be starved, eliminating all sources of sugar from the diet won’t kill them. The fundamental food source for all cells, including cancer cells, is glucose. In a cancer patient, metabolic changes can induce the body to disintegrate body fats and lean body mass to produce energy for both cancer cells and healthy cells. Regardless of sugar intake, this is the case. It may be essential to stay away from foods high in simple sugars if the person experiences problems with watery diarrhoea after consuming such foods. The foods that are high in simple sugars contain rich desserts, ice cream, sweetened drinks, candy, and fruits packed in syrup.
If a cancer patient is facing weight loss not related to blood sugar control, it may be due to cancer-induced weight loss, called cancer cachexia. In this condition, the breakdown of body fat and lean body mass is a result of chemical changes in the body, which produce energy for both cancer and healthy cells. Another supplement might need to be added to the diet. The best supplement for you will depend on your doctor or dietitian.

The Impact of Diabetes Management on Pancreatic Cancer Risk:
Keeping diabetes under control is crucial for reducing the risk of pancreatic cancer and other diabetes-related complications. Lifestyle modifications, such as maintaining a healthy weight, engaging in regular physical activity, and following a balanced diet, are essential components of diabetes management. These measures not only improve blood sugar control but may also lessen the risk of developing pancreatic cancer.
Medications used to treat diabetes have also been examined for their potential influence on pancreatic cancer risk. Some studies suggest that the use of metformin, a common diabetes medication, may reduce the risk of pancreatic cancer, while other medications, such as insulin and sulfonylureas, may increase the risk. However, the evidence is not yet conclusive, and further research is needed to understand the impact of diabetes treatment on pancreatic cancer risk.

Diabetes as a Consequence of Pancreatic Cancer:
While diabetes condition can be a risk factor for pancreatic cancer, it can also be a consequence of the disease. As pancreatic tumours grow, they may interfere with the pancreas’s ability to produce insulin, leading to diabetes. This secondary diabetes is often characterized by a rapid and unexplained onset of high blood sugar levels, which can be challenging to control with standard diabetes treatments.
For patients with unexplained, sudden-onset diabetes, especially those over 50 years of age, healthcare providers may consider screening for pancreatic cancer, mainly if there are other symptoms, such as unexplained weight loss or jaundice.
Conclusion:
Diabetes and pancreatic cancer are complicated in their relationship, with diabetes serving as both a risk factor and a potential symptom of the disease. Understanding this connection is crucial for early detection and prevention efforts. Patients with long-standing diabetes should be aware of the increased risk and maintain regular follow-ups with their healthcare providers. Similarly, individuals with new-onset diabetes, particularly older adults, should be monitored closely for any signs of pancreatic cancer. As research continues, the hope is that improved screening methods and a deeper understanding of the diabetes-pancreatic cancer link will lead to earlier diagnosis and better outcomes for patients at risk.